Percutaneous Lumbar Disc Laser Decompression
Percutaneous lumbar disc laser decompression is a minimally invasive surgical procedure used to treat lumbar disc herniation, a common cause of low back pain and radiating leg pain (sciatica). This technique is especially effective for patients who have not responded to conservative treatments. The procedure involves using a laser to shrink the herniated portion of the disc, relieving pressure on the spinal nerves and reducing pain.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar disc herniation is one of the most common causes of low back pain, affecting people in their 30s to 50s. It is particularly prevalent among individuals who perform repetitive physical activities, heavy lifting, or those with a history of trauma to the spine. The condition is more common in the lumbar spine because this area bears the majority of the body’s weight. Percutaneous lumbar disc laser decompression is typically recommended for patients who have failed to benefit from at least 6 weeks of conservative treatments.
Why It Happens – Causes (Etiology and Pathophysiology)
A lumbar disc herniation occurs when the nucleus pulposus (the soft, gelatinous center of the intervertebral disc) protrudes through a tear in the annulus fibrosus (the tough outer layer of the disc). The herniated disc may compress spinal nerves or the dural sac, leading to symptoms such as pain, numbness, tingling, and weakness in the lower back, legs, or feet. Factors that contribute to disc herniation include:
-
Degenerative Disc Disease: The natural wear and tear of spinal discs over time.
-
Traumatic Injury: Sudden impact, lifting, or twisting motions can cause the disc to rupture.
-
Repetitive Stress: Overuse or improper lifting techniques may cause disc material to herniate.
-
Age: As people age, their discs become less hydrated and more prone to damage.
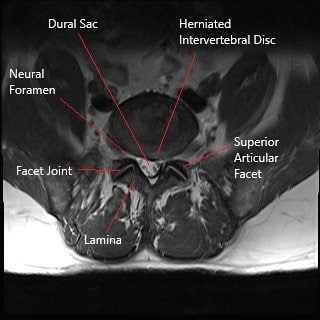
Axial section section of lumbar spine showing herniated intervertebral disc.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae (L1-L5) and the intervertebral discs between them. These discs act as shock absorbers, allowing for movement and flexibility. The spinal cord runs through the spinal canal, and nerves branch off from the cord through openings between the vertebrae, known as foramina. These nerves control sensations and movements in the lower back, legs, and feet. A herniated disc can compress these nerves, leading to symptoms like pain, numbness, and muscle weakness.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of a herniated lumbar disc include:
-
Low Back Pain: Often sharp or aching, localized in the lower back.
-
Radiating Pain: Pain that travels down the legs (sciatica), typically on one side.
-
Numbness or Tingling: In the legs, feet, or toes, caused by nerve compression.
-
Weakness: Difficulty gripping or lifting objects, and loss of strength in the legs or feet.
-
Pain Aggravated by Movement: Symptoms often worsen with activities like bending, twisting, or sitting for long periods.
How Doctors Find the Problem? (Diagnosis and Imaging)
To diagnose a herniated disc, doctors typically use:
-
Physical Examination: Assessing reflexes, strength, and pain response to identify nerve root involvement.
-
MRI (Magnetic Resonance Imaging): The preferred imaging technique to visualize disc herniations, nerve compression, and inflammation.
-
CT (Computed Tomography) Scan: Provides detailed images of bones and may be used in conjunction with MRI for further evaluation.
-
X-rays: Help rule out fractures, arthritis, or spinal alignment issues.
-
Electromyography (EMG): Measures nerve function to confirm compression of the spinal nerves.
Classification
Percutaneous lumbar disc laser decompression is typically used for:
-
Single-Level Disc Herniation: Involving one disc in the lumbar spine.
-
Multi-Level Disc Herniation: Rarely, laser decompression can be used for multiple herniated discs if indicated.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic the symptoms of lumbar disc herniation include:
-
Spinal Stenosis: Narrowing of the spinal canal causing pressure on the nerves.
-
Sacroiliac Joint Dysfunction: Dysfunction in the joint between the sacrum and pelvis, often causing low back and leg pain.
-
Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle in the buttocks.
-
Facet Joint Syndrome: Degeneration of the facet joints, which can cause pain similar to sciatica.
Treatment Options
Non-Surgical Care
-
Physical Therapy: Strengthening the muscles that support the spine and improving flexibility.
-
Medications: Pain relief from NSAIDs or corticosteroids, as well as muscle relaxants for spasms.
-
Epidural Steroid Injections: To reduce inflammation around the affected nerves.
-
Nerve Root Blocks: For targeted pain relief.
Surgical Care
-
Percutaneous Lumbar Disc Laser Decompression: A minimally invasive surgery using laser energy to shrink the herniated disc and relieve nerve pressure.
-
Microdiscectomy: A traditional surgical option to remove the herniated disc material.
-
Spinal Fusion: In cases where the spine requires stabilization after disc removal.

Intraoperative image of lumbar microdiscectomy surgery.
Recovery and What to Expect After Treatment
Post-operative recovery from laser disc decompression typically involves:
-
Pain Management: Minimal post-operative pain due to the minimally invasive nature of the procedure.
-
Physical Therapy: Gradual strengthening and flexibility exercises.
-
Outpatient Procedure: Most patients are discharged the same day as the surgery.
-
Activity Restrictions: Avoid heavy lifting and high-impact activities for a few weeks.
Possible Risks or Side Effects (Complications)
While percutaneous lumbar disc laser decompression is generally safe, there are potential complications, including:
-
Nerve Damage: Risk of injury to the nerve roots or spinal cord during the procedure.
-
Infection: Although rare, infection at the incision site may occur.
-
Spinal Injury: The laser energy may cause damage to the vertebral bodies or spinal nerves if not properly controlled.
-
Inadequate Decompression: The disc may not shrink enough, leading to continued symptoms.
-
Recurrence of Herniation: In some cases, the disc may herniate again, requiring additional treatment.
Long-Term Outlook (Prognosis)
The prognosis after laser disc decompression is generally favorable, with most patients experiencing significant pain relief and a return to normal activities. However, some patients may experience recurrence of the herniated disc, and in those cases, additional treatment or surgery may be needed. Long-term success rates for laser decompression are comparable to traditional microdiscectomy, though microdiscectomy is still considered the gold standard in some cases.
Out-of-Pocket Cost
Medicare
CPT Code 62287 – Percutaneous Lumbar Disc Laser Decompression: $137.26
Under Medicare, 80% of the approved cost for this procedure is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved procedures like percutaneous lumbar disc laser decompression. These supplemental plans work directly with Medicare to provide full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar disc condition requiring laser decompression surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, imaging, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar disc herniation or injury requiring laser decompression is caused or worsened by a motor vehicle accident, No-Fault Insurance will cover the full cost of necessary procedures. The only possible out-of-pocket expense may be a small deductible depending on your individual policy terms.
Example
Rachel, a 54-year-old patient with a lumbar disc herniation, underwent percutaneous lumbar disc laser decompression (CPT 62287) to relieve sciatica and nerve compression. Her estimated Medicare out-of-pocket cost was $137.26. Since Rachel had supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. How long does it take to recover from laser disc decompression?
A. Most patients experience significant pain relief and can return to normal activities within 1-2 weeks. Full recovery may take a few weeks to a month, depending on the individual.
Q. Is laser disc decompression successful for everyone?
A. Laser decompression is highly effective for most patients with single-level disc herniations. However, it may not be suitable for those with multi-level herniations or severe spinal instability.
Q. Are there risks associated with the laser technique?
A. While the procedure is minimally invasive, there are risks such as nerve injury, infection, or incomplete decompression. These risks are low but should be discussed with your surgeon.
Summary and Takeaway
Percutaneous lumbar disc laser decompression is a minimally invasive option for treating herniated discs and relieving symptoms like pain and numbness in the legs. It is a safe and effective procedure, offering faster recovery and fewer complications compared to traditional open surgery. However, it is not suitable for all patients, and a thorough consultation with a spine specialist is necessary to determine if it is the right treatment.
Clinical Insight & Recent Findings
Who Performs This Treatment? (Specialists and Team Involved)
Laser disc decompression is typically performed by:
-
Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal conditions.
-
Anesthesiologists: For anesthesia management during the procedure.
-
Physical Therapists: To assist with post-operative rehabilitation.
When to See a Specialist?
If you experience persistent lower back pain, sciatica, or other symptoms of a herniated disc that don’t improve with conservative treatments, consult a spine specialist to discuss your treatment options.
When to Go to the Emergency Room?
Seek emergency care if you experience:
-
Sudden loss of bladder or bowel control.
-
Severe pain that does not respond to medications.
-
Sudden weakness or numbness in the legs or feet.
What Recovery Really Looks Like?
Recovery is generally quick, with most patients experiencing significant relief within weeks. Physical therapy and activity modifications are crucial during the recovery period to ensure lasting results.
What Happens If You Ignore It?
Ignoring symptoms of a herniated disc can lead to worsening pain, permanent nerve damage, and decreased mobility. Early intervention often leads to better outcomes and faster recovery.
How to Prevent It?
Maintaining a healthy weight, practicing good posture, and engaging in regular back-strengthening exercises can help prevent disc herniation and reduce the need for surgery.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D supports bone health, and regular exercise helps maintain spinal integrity, reducing the risk of disc problems.
Activity and Lifestyle Modifications
After surgery, it is important to avoid heavy lifting and high-impact activities during recovery. Light activities such as walking or swimming can help strengthen the back and improve flexibility.
Do you have more questions?
What is a herniated disc?
A herniated disc occurs when the soft, gel-like center (nucleus pulposus) of an intervertebral disc pushes through a crack in the tough outer layer (annulus fibrosus).
¿Qué es una hernia discal?
Una hernia discal se produce cuando el centro blando y gelatinoso (núcleo pulposo) de un disco intervertebral empuja a través de una grieta en la dura capa externa (anillo fibroso).
What causes a herniated disc?
Herniated discs can result from degenerative disc disease, trauma, repetitive stress, or heavy lifting.
What non-surgical treatments are available for a herniated disc?
Treatments include physical therapy, NSAIDs, activity modification, heat/cold therapy, nerve root blocks, and epidural steroid injections.
What are the symptoms of a herniated disc?
Symptoms include low back pain, sciatica, numbness, tingling, and weakness in the legs.
When is surgery considered for a herniated disc?
Surgery is considered when non-surgical treatments fail after at least six weeks or if there is severe nerve compression causing significant symptoms.
What is laser disc decompression?
Laser disc decompression is a minimally invasive procedure that uses laser energy to shrink the nucleus pulposus, relieving pressure on the nerves.
When is surgery considered for a herniated disc?
Surgery is considered when non-surgical treatments fail after at least six weeks or if there is severe nerve compression causing significant symptoms.
What non-surgical treatments are available for a herniated disc?
Treatments include physical therapy, NSAIDs, activity modification, heat/cold therapy, nerve root blocks, and epidural steroid injections.
How is laser disc decompression performed?
Under local anesthesia, a needle and fiber optic are inserted into the disc using fluoroscopic guidance. Laser energy is then applied to shrink the disc material.e
What is the recovery like after laser disc decompression?
Most patients can go home the same day and experience significant pain relief, though they should avoid strenuous activities during recovery.
What are the risks of laser disc decompression?
Risks include thermal damage to nearby structures, inadequate shrinkage of the disc, and potential injury during needle insertion.
How does nucleoplasty differ from laser disc decompression?
Nucleoplasty uses radiofrequency energy instead of laser energy, generating less heat and reducing the risk of thermal damage.
What are the benefits of microdiscectomy over other procedures?
Microdiscectomy allows for precise removal of the herniated disc material, making it the gold standard for herniated disc surgery.
What is microdiscectomy surgery?
Microdiscectomy is a surgical procedure where the herniated disc material is removed under direct vision using an operating microscope.
What are the risks of microdiscectomy surgery?
Risks include infection, bleeding, nerve damage, and recurrence of the herniation.
How long is the recovery after microdiscectomy surgery?
Recovery time varies, but most patients can return to normal activities within a few weeks to a few months.
Can a herniated disc heal on its own?
In some cases, herniated discs can heal with conservative treatment over time, but severe cases may require surgery.
What is cauda equina syndrome?
Cauda equina syndrome is a serious condition where severe compression of the nerve roots in the lower spine causes loss of bowel or bladder control and leg weakness, requiring immediate surgery.
Is it possible to prevent a herniated disc?
Preventative measures include maintaining good posture, regular exercise, proper lifting techniques, and avoiding excessive strain on the back.
How do I know which treatment is best for my herniated disc?
The best treatment depends on the severity of symptoms, response to non-surgical treatments, and overall health. Consulting with a spine specialist can help determine the most appropriate treatment.
What lifestyle changes can help manage a herniated disc?
Lifestyle changes include staying active, losing weight if overweight, avoiding prolonged sitting, and strengthening the core muscles.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
